5 patients. 1 doctor. 1 MODERATOR. 1 Goal.ADDRESS PAIN INEQUITY AT THE SOURCE
In this roundtable discussion, we'll share painful truths that validate systemic pain bias and empower the world to advocate for change.
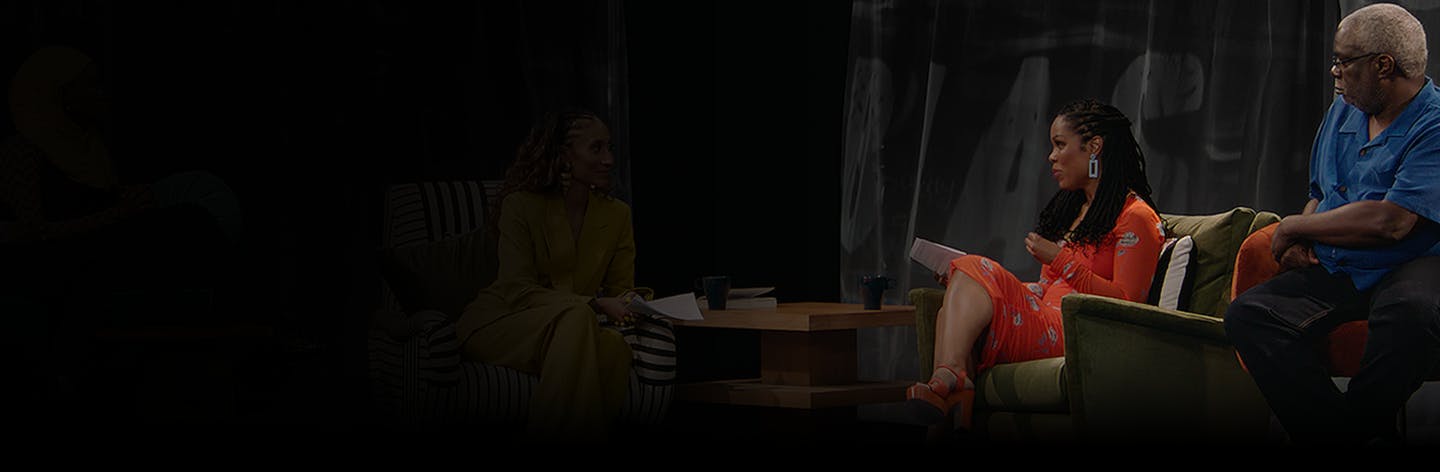
The Believe My Pain ROUNDTABLE
-
Part 01
The Reality of Pain Inequity
Learn what pain inequity is and how inequitable treatment impacts Black communities.
-
Part 02
True Stories of Pain Bias
Hear from 5 Black patients who have personally experienced pain bias in healthcare.
-
Part 03
The History of Pain Inequity
Uncover the sources of pain bias, including perpetuated myths and beliefs.
-
Part 04
Solutions for Pain Equity
Discover perspectives on preventing and overcoming inequitable pain experiences.
Derek:
When I approach a medical professional, I'm frustrated that we have to validate our pain just to get treated like human beings.
Deidra:
The healing of the body was easy for me. It's the psychological part. It’s awful.
Etisyai:
I should not have to beg my doctor to run tests or ask them to take another look.
Elaine:
Welcome to believe my pain, A discussion about systemic pain bias in health care. I want to thank all of you and all of you for joining me today as we talk about this very important issue. I also want to thank The Advil Pain Equity Project developed by Advil in partnership with the Morehouse School of Medicine and BLKHTLH for inviting us to be a part of their commitment to addressing pain bias in black communities.
Elaine:
All right. Let's get right into it with our first topic, the reality of pain inequity.
Elaine:
Pain equity is achieved when everyone is treated equally, regardless of their age, race, ethnicity, gender, or socioeconomic status, and receives the highest quality pain care and management. Okay. So Dr. Uché, you have written this book, Legacy: A Black Physician Reckons with Racism in Medicine.
Elaine:
You are a legacy black female physician and you are armed with expertise that frames this issue around black pain in such a clear way. And so I'm so glad that you're here today. Thank you for being here.
Dr. Uché:
Thank you. Thank you for having me. I'm so excited to be here to talk to you about this issue that means so much to me and impacts so many members of our community. And we'll hear those stories today.
Elaine:
All right. So, Doctor Uché, could you just outline what are some of the myths about black people in pain?
Dr. Uché:
So I think, like, the main thing is that health professionals think that black people are biologically different than other people, that our skin is thicker, that we have less sensitive skin and higher pain tolerance. And that is all absolutely false. There is no difference between black patients and patients of other races.
Elaine:
Wow. So what do you think is perpetuated these myths?
Dr. Uché:
You know, the legacy of slavery in this country. I think interpersonal and systemic racism that still exists in this country and that is embedded into the institution of medicine and health care. You know, our health professionals, most want to do a good job and care for their patients. But unfortunately, we're seeing implicit bias that they are not listening to their patients, they're not responding to their patients concerns. And sometimes even ignoring their patients.
Elaine:
And the only way that we can expose and address it is by first telling our stories. We want to work better with doctors. And we, and I think that a better, healthier medical system actually allows doctors to do their job better.
Dr. Uché:
Agreed
Elaine
To truly relieve pain, we need to put an end to systemic bias and to believe black people when they say, t hey're in pain.
Elaine
What we're all here to talk about is something that we have in common, which is not being believed, not having our pain taken seriously. And each of you represent a much bigger medical phenomenon, frankly, that needs to be exposed and addressed, and it's an issue around pain inequity. Just to characterize this issue of pain and equity. I just want to share a stat that I think will resonate with all of you.
Elaine
It's from an Advil study on pain equity, and it says this, “among black people suffering from pain, three in four say they believe there's bias in how pain is diagnosed and treated. 74%. So I share these stats to underscore that you are not alone in what you have experienced. And that's why we're here to to validate your stories.
Elaine
So Etisyai. you too have experienced your pain being dismissed within the medical system. Tell us your story.
Etisyai
So at age 14, I had already started experiencing excruciating menstrual cramps. I would go to the doctor and I would tell them all my symptoms and they would just be like, you know, it's just a period, you know, that's just how it goes. You're just a woman, you know, this is what women have to go through. You know, you're you have to be strong because this is not going to end until you hit menopause.
Etisyai
And it's just like, why are you trying to minimize what I'm experiencing by saying that this is what women go through? This is not what women have to go through. I moved down to Florida April 9th, and ten days later I was in emergency surgery. But when they went in there, they saw so much damage. And now I'm dealing with the consequences of the negligence that I've been facing all these years.
Etisyai
They had to remove my left ovary. They had to remove my fallopian tube and, you know, the damage was already done. So it's kind of like, was it on me because I wasn't going to the right doctors or is it that you guys are not paying attention and you just don't care about the pain that I'm experiencing? And I really do feel like it was the latter.
Elaine
This is a case where you did everything right. Thank you for sharing.Mark, I'd love to hear you share a little bit of your story. I know you you went into the E.R. with chest pain.
Mark
This started one morning and I woke up and I just tried to breathe. It just felt weird when I was trying to breathe. So I finally went into the emergency room, and their initial observation was they couldn't find out what was wrong with me. So they sent me back home, said just take some over-the-counter medicine, went home. I just kept getting worse and worse and worse.
Mark
So then I go to the emergency room. They couldn't find anything that was wrong with me. They sent me back home again and I got worse and worse. At this time. I just needed the help of anybody and I just felt like I was being lost and left behind. I got to the point where I it was the final day where I thought, this is gonna be my last day on Earth because my breathing was just terrible.
Mark
And like, I could feel my heart slowing down. I had my son and his mom, they had went to another location because I didn't want to get sick with whatever I had. So I called her and I said, I need to speak to my son. And she said, Why? I said, I just want to tell him goodbye one last time and that I love him.
Mark
And I didn't know I was if I was gonna get a chance to see him grow up any further, I wasn't gonna be there to talk to him about women and how to date you know, how to navigate through life. The different things that you may come in contact with, the conflicts and all that. And his mom said, No, we're coming to get you. And they rushed me to the hospital.
Mark
They said, well let's let's check out his heart. Then they found out I did have fluid coming around my heart and it was called pericarditis. And they sent me to a cardiologist and I was telling them what I was feeling. And he kept saying, no, I don't think you're feeling that.
Mark
It couldn't possibly be that. And I basically had to beg my doctor to do bloodwork because that's how they found out that I had an inflammation in my heart the first time. He was reluctant to do the blood work, but I kept pushing and kept pushing like, Look, please do the blood work. He finally did it and it was at this point, I'm like, this whole time, I think I'm going crazy, but I know something is going wrong.
Mark
Nobody's listening to what I'm telling you is going wrong. And I just want you to hear that I'm telling you. I know my body. I know what I feel. You can't tell me what I feel, but something is wrong. They just wouldn’t listen to me. And it was, it was aggravating, thinking like, I don't want to leave this Earth and not see my son again.
Mark
I won't leave this Earth knowing I have so much more I want to do. But I thought I was going to be leaving this Earth at that point.
Elaine
You said that you got to the point where you thought it was the end for you and you thought that you weren't going to survive it. But you did survive it and you're here to tell your story. So many heads are nodding because we all have experienced some some portion of that. I'm sure. Deirdre, I'd love to talk to you next.
Elaine
So your sixth pregnancy you’re experiencing chest pain.
Deidra
When I went to the hospital, I gave a normal birth. Everything was fine. And then afterwards I was like I was having a lot of chest pain, like heaviness. I didn't know how to describe it. And I was telling the nurse, I said, I was like, I don't feel right like something feels very weird in my chest.
Deidra
She was like, Oh, well, when you when you go home, everything will be okay. So when I went home, we was carrying stuff up the stairs and I felt like a, like a pressure in my chest, like something I kid you not. It felt like something tore, My grandfather was like, I think we should go call another doctor.
Deidra
And they came and did an EKG. They was like, the EKG is abnormal. I was like okay, so they did an ultrasound on my heart. It was like well you have a leaking valve and everything. So I was like, okay, my troponin levels was very high. He was like that means you having a heart attack. I was like, I'm sitting here talking to you.
Deidra
There’s no way I'm having a heart attack. I just left the hospital from having a baby. What happened was my artery tore and it flapped over, so it stopped all the blood from properly flowing through. So it was it was a very scary experience, obviously.
Elaine
So you had a heart attack?
Deidra
Yeah.
Elaine
I’m so sorry. As a mom, this story really resonated with me a lot. All right, so, Derek, let’s go with you next. I would love to hear your story.
Derek
I've had migraines since I was ten and for a long while, people believed men didn't get migraines. It got so bad, I drove myself to the emergency room. And this doctor comes in, little woman, and she looks at me, “Oh big men don't get migraines. You sure it's a migraine?” And she's just arguing with me that I don't have a migraine.
Derek
And I threw up on her. Oh, All of a sudden, they're flying around, getting me the drugs and everything that I need to stop my migraine. We shouldn't have to fight that hard to be taken care of. It's both the skin color and the size. You know, you don't feel that they diminish what I'm going through.
Derek
So now I go to a medical. When I approach a medical professional, we're at war. I'm coming in knowing I got a fight you.
Elaine
Don't accept what they tell you. Follow your instincts and keep advocating for yourself. Hearing these stories arms us with tools and with a different protocol, a different way to navigate them. So thank you for sharing that.
Elaine
Inaayah you were diagnosed with sickle cell?
Inaayah
Yes, I have. I was diagnosed with sickle cell anemia at birth.
Elaine
So you have learned how to navigate life with sickle cell anemia, with chronic pain. Your whole life?
Inaayah
Yes, we call it flare ups. So around two years ago, I started experiencing one of my flare ups. I went to the emergency room and I told them all of my symptoms, you know, just like very upset and crying and, you know, because I was feeling so much pain. So the nurse called me in, she sees that I'm visibly, you know, in pain and she's like okay
Inaayah
I'm going to, I'm going to try to get the doctor right away. You know, she was she was very sympathetic. She asked me of my pain level and I told her ten out of ten she was okay. Okay. So what usually works for you? So she was like okay I'll go bring the doctor in and I'll tell him. So upon coming in
Inaayah
He didn't even say, you know, greet himself. So you say your pain level is a ten out of ten how are you talking right now? He was trying to be petty with it. Like he wasn't being sympathetic at all. He was like, if it was a ten out of ten, you wouldn't be talking. So you really should say nine out of ten.
Inaayah
And he was like, first of all, I just know that I'm not going to give you that amount of pain medicine. And he's talking about two milligrams. It's like one I.V. shot. So the nurse, she literally just butted in and she was like listen. She was like don't you see that this girl is in pain. She was like the record say that she's taken this before.
Inaayah
I looked at her records. You haven’t even looked at her record. The doctor was white and the nurse was also white and when she was talking to him, he was looking at her in her eyes. He was he seemed more receptive, receptive to her telling my story than me telling my own story. So after that, he would just say, okay, fine, order it from the pharmacy and see if they approve it. She was like you know that they're going to approve it.
Inaayah
Me my mom and my sister had been crying, talking to him for like the past 30 minutes. And she talked to him for maybe like 5 to 10 minutes. And he he he approved it even unwillingly and just walked out of the room and she was able to give me the medicine.
Elaine
I'm so sorry that you've had to go through that. It’s not normal. It is common and it is not normal. So, Dr. Uché, after hearing all of these experiences, what do you think this tells us about the state of the medical system as we know it?
Dr. Uché
Yeah, this tells us clearly that our health care system is in dire straits and it is broken. So we have to do work on educational level, on a protocol level within hospitals and health care institutions, and think about strategies for increasing diversity among health professionals.
Elaine
We are not anti doctor. No, none of us up here are anti doctor. We recognize that doctors have an essential place in our society. What we are acknowledging is that the system in which doctors work is broken, it's sick, it needs healing, it needs help so that doctors can do what they were put there to do, which is care for people like us.
Elaine
With that, I'll just say I think, you know, with all of us coming together, I think it's an indication that if we continue to work at this, the day will come when pain inequity will be a thing of the past. I believe that I believe it's possible in our lifetime. But we can't we can't silence ourselves and we can't give up the fight.
Elaine
So Dr. Uché, Derek, Mark, Deirdre, Inaayah, Etisyai thank you so much for being here.
Elaine
Black people in this country are burdened by our history. This lived experience of oppression and bias in the medical system has been really unconscionable.
Elaine
This is something that has been happening since we were brought here as a people. And so I'd love to sort of hear from you about the historical framework around black pain.
Dr. Uché
It literally is embedded into the essence of medicine. During slavery, we had actual physicians, people who were revered, who were respected, coming up with technology and innovations, but doing it in such a horrific way in a way that dehumanized black people. J Marion Sims. He was known as the father of modern gynecology, and he made some really important advances in obstetrics and gynecology.
Dr. Uché
And he did so by experimenting on enslaved black women who could not give consent. One woman in particular, he performed 30 procedures on
Elaine
My God.
Dr. Uché
Another surgeon and psychologist named Samuel Cartwright. Again, very, very respected. But coming up with this idea that black people had more sensitive skin, more sensitive nervous systems, perpetuating and embedding these myths into the foundation of medicine.
Elaine
So dangerous. So dangerous.
Dr. Uché
We had medical students and residents believing that there are biological differences between black patients and other patients. And so even that was perpetuated, even more post, you know, post-Civil War reconstruction when black people, even though they were free, were still being used for experimentation.
Elaine
That is very grave.
Dr. Uché
So going on from 1900s to 19- 1970s. Right. So these involuntary sterilization programs. Some of them were known as the Mississippi appendectomy. So sometimes people would go in for a procedure, think they're getting one procedure, then something else happened. So, for example, the Relf sisters, they were only 12 and 14 years old. Their mom was told that they were getting a shot, you know, for birth control, but instead they were surgically sterilized.
Dr. Uché
So that's where the whole idea of, you know, informed consent is so important. Even, you know, we'll talk about the Tuskegee experiment. You know, those were men in rural Alabama who were didn't have a formal education. They were given lunch money, bus money to enroll in a study that the U.S. Public Health Service funded. And so they all had syphilis, but they were just told they had bad blood.
Dr. Uché
They weren't told exactly what they had. And even once treatment had become available, penicillin, they were not given that treatment because the whole goal of the study was to see what would happen if someone who was infected with syphilis, what would happen if you left it untreated? Right. But again, informed consent was not obtained. But I think there was no trust to begin with.
Elaine
Oh, my gosh.
Dr. Uché
To think about our own federal government funding these programs. And the only reason that the Tuskegee experiments ended was because a black epidemiologist found out about it and alerted the Associated Press in the 1970s.
Elaine
And today were asked to just trust doctors blindly.
Dr. Uché
In current day, people are still having experiences where they're silenced or they're spoken over.
Elaine
And unfortunately, these experiences are happening to black people of every socioeconomic background, at every education level.
Dr. Uché
Even with my medical degree, I am more likely to die of pregnancy related complications than a white woman with an eighth grade education. I'm also more likely to die than my mom was during pregnancy. Like, how does that how does that make sense?
Elaine
It doesn't.
Dr. Uché
You know, it just is so incredibly disturbing. It's the motivation for why I do the advocacy work that I do, why we're sitting here right now.
Elaine
It's really chilling to hear you string together this historical timeline of how black people's pain has been ignored or how black folks have been abused, frankly, by the medical system throughout time.
Dr. Uché
I think it's so important that health care institutions like the CDC are making sure that they get this information out to the general public.
Elaine
Thank you so much, Doctor Uché for just being here today and sharing this knowledge with all of us.
Dr. Uché
Thank you, Elaine
Elaine
It means a lot as we continue to strive for pain equity, It's important to remember the sources of our pain to ensure this type of treatment stays in the past.
We have a medical professional here who is working towards solutions every single day.
So, Doctor Uché, what do you think this tells us about the state of the medical system?
As we know it?
This tells us clearly we have a lot of work to do within this system.
So we have to do work on an educational level, on a protocol level, within hospitals and healthcare institutions, and think about the strategies for increasing diversity among health professionals.
You know, we talk about trainings and I think trainings are very very important.
That is a starting point, so anti-racism trainings, implicit bias trainings are important
But we know that that's not enough.
And so I think other things that need to happen is accountability. Healthcare professionals, you know, need to be part of a system where there are protocols in place to mitigate that bias.
And so what does that look like?
It looks like making sure that for every health care professional, someone and authority is keeping track of how they're treating pain.
We need every health professional to speak up when they see these these situations happening.
It's unacceptable not to.
We want to work better with doctors, and I think that a better, healthier medical system actually allows doctors to do their job better.
Advil has begun to work at the educational level, launching a certified course for the next generation of healthcare professionals.
The Advil Pain Equity Project course aims to provide future physicians and healthcare professionals with the knowledge, tools, and resources to understand and address racial health inequities and pain prevention, treatment, and management.
Another part of the solution is to ensure protocols and assessments are in place that mitigate bias and feel created.
Advil created tools and resources to help black patients
educate and advocate for themselves.
When you hear solutions that you can seek out, it empowers you to make a different decision, a better decision for you.
I'm hopeful that if we keep putting our heads together to find solutions and continue being advocates for ourselves and our communities, we'll eventually get to a time of true pain, equity.
MORE FROM THE ROUNDTABLE
Sign up to receive notifications when additional parts from The Believe My Pain Roundtable go live.
Meet our MODERATOR, HEALTHCARE PROFESSIONAL AND DIRECTOR

Elaine Welteroth
Elaine Welteroth is an award-winning American journalist, New York Times bestselling author, former editor-in-chief at Teen Vogue, seasoned television producer and host, and a new voice in the fight for Black maternal health in America.

DR. UCHÉ BLACKSTOCK
Dr. Uché Blackstock is a physician, thought leader, and sought-after speaker on bias and racism in medicine and health care. Dr. Blackstock founded Advancing Health Equity in 2019 with the goal of partnering with healthcare organizations to dismantle racism in healthcare and to close the gap in racial health inequities.

BETHANY MOLLENKOF
Bethany’s directing work uses a thoughtful approach to tell complex stories about gender, culture, identity, and self-representation. Her process often uses found imagery, archives, written narratives, and photography. In 2022, Bethany’s first film premiered at the Tribeca Film Festival. Her work has been featured in the Super Bowl, she is a Neiman Fellow at Harvard and was voted one of the top 30 photographers of 2022.